Todays post is about Fibromyalgia.
A topic that has been discussed a bit in my family of late.
This is a fairly common condition that affects many people, from all walks of life. Statistically it affects women more than men.
So, what is Fibromyalgia?
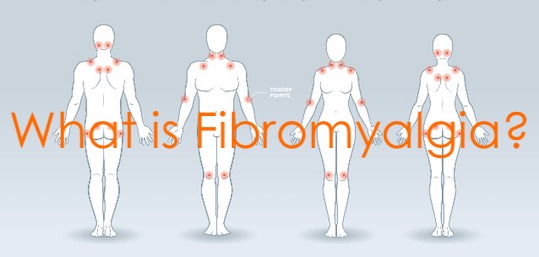
As described in Davidson’s Principles & Practice of Medicine; fibromyalgia is a condition that presents as widespread body pain, which is often worse in the neck and back.
People who suffer from the condition have a reduced pain threshold and tenderness at certain sites throughout the body. Many sufferers find that physiotherapy often makes it worse. These symptoms are often accompanied by fatigue; memory problems and disturbed sleep patterns. A high proportion of fibromyalgia patients also suffer from tinnitus.
Fibromyalgia commonly begins between the ages of 35 and 50 years of age.
What causes it?
The cause is poorly understood, however there are 2 factors that are thought to be major contributors.
Poor sleep, or more exactly, reduced non-rapid eye movement (non-REM) sleep.
Delta waves are characteristic of deep stages of non REM sleep. This usually occurs in the first few hours of sleep. This type of sleep is recognised as having an important restorative function.
The other factor is thought to be psychological distress, such as anxiety or distressing life events.
Unfortunately, the condition can also create a perpetual cycle.
– The pain causes anxiety and poor sleep – the anxiety and poor sleep contribute to the condition causing pain – and so the cycle repeats.
How is it diagnosed?
Fibromyalgia is a complex condition that has many varied symptoms that could also be linked to other health problems. There are no blood tests or imaging test that show this condition, so it is difficult to diagnose.
Therefore most health professionals will have to conduct various tests to rule out conditions with similar symptoms.
How is it treated?
There are no guaranteed cures or medications for fibromyalgia. The most recent research I could find recommends a combination of treatments. This is to help patients manage the individual factors contributing to the condition.
The most common of these are pain, sleep, physical activity and psychological wellbeing.
Most treatment programs seem to include simple measures such as hot baths, aerobic and strength exercises along with relaxation and meditation.
The studies surrounding this condition, the causes and the treatments are ongoing.
I hope that this information is helpful to you or anyone you may know with this condition.
Till the next post,
Live clean n prosper.
Sources – Davidson’s Principles & Practice of Medicine, hindawi, science direct, Pub Med